In today’s edition of Glen Abbey’s Physiotherapy blog post we are going to discuss cervical spondylosis (Spon-du-low-sis). Throughout the blog we will be discussing the definition, incidence rate, etiology, differential diagnosis, the effects and causes of cervical spondylosis, the clinical presentation and treatment of the condition. Here at Glen Abbey physiotherapy we commonly see neck conditions in both older and younger individuals, however this condition is seen in roughly 25-35% of our neck injuries in individuals above the age of 45, therefore we believe it would be best for our patients to learn a bit about their condition before seeing their physiotherapists here or referring a friend of family member to see one of our registered physiotherapists.
What is Cervical Spondylosis?
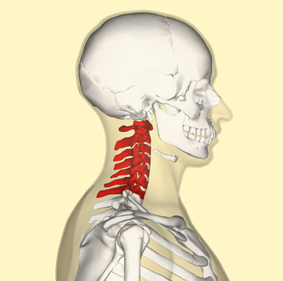
There is a common theme with this condition, our patient comes in for an initial assessment with an x-ray report stating ‘I have some sort of spinal disease’. The condition of cervical spondylosis may be very confusing at times because of the fair number of synonymous terms with the condition. On your x-ray you may read one of the following words depending on which x-ray technician read your report and their level of schooling: degenerative disc disease, segmental instability, hypertropich arthritis, degenerative spondylosis, cervical arthrosis, osteophytosis, spondylitis deformans, cervical spondylathritis, cervical spondylarthrosis, cervical osteoarthritis, and cervical arthrosis. The majority of the time, the most common synonymous term with cervical spondylosis is degenerative disc disease. You may also see this condition written down by your family doctor as ‘DDD’. So what exactly is this condition? Spondylosis is an inflammatory and degenerative condition of the cervical spine, which results in the degeneration of the cervical mobile segment. Cervical simply means the portion of your spine, which makes up your neck, roughly from the base of your hair line to the collar of your shirt. In laymen’s terms, cervical spondylosis is simply neck inflammation and wear and tear.
Read More About Cervical Spine DDD Here
Who Develops Cervical Spondylosis?
Now that we know what the condition is and how to spot it on a referral prescription or on x-ray, lets gain some insight into why this condition is so commonly seen by our physiotherapists at Glen Abbey physiotherapy. Roughly 60% of individuals over the age of 45, 85% of those over the age of 65 and 90% of those over the age of 70 will show some form of cervical spondylosis and degenerative disc disease in their neck at at least one of their 7 cervical segments. It is most commonly seen as the cervical segments involving the 5th and 6th, followed by the 6th and 7th. It is the most severe at the levels where movement is the greatest. There is much controversy over whether or not cervical spondylosis is an inevitable degenerative process, which occurs with aging, or whether these degenerative changes are the result of trauma, poor postural habits or genetic weakness. The presence of cervical degenerative disc disease is usually seen in correlation with a medical history of a herniated disc, post laminectomy, post discectomy, post cervical fusion, cervical vertebrae fractures, cervical infections, tumors, spondylolisthesis and scoliosis. Often this condition results from a combination of etiologies including congenital factors, smoking, circulatory factors, biomechanical effects and direct or indirect trauma or micro trauma.
Before you begin to diagnose yourself with Dr. Google, it is best to understand that there are many different conditions that mimic a presentation of neck degenerative disc disease. The presentation of a patients condition may be neurologic (multiple sclerosis, amyotrophic lateral sclerosis, cervical cord tumors, peripheral nerve entrapment neuropathies, brachial plexus neuritis and thoracic outlet syndrome), inflammatory (rheumatoid arthritis, fibrositis, polymyalgia rheumatic), neoplastic (tumors), shoulder or upper extremity conditions – most often the differential diagnosis of cervical spondylosis (subacromial impingement, calcific tendinitis, biceps tendinitis, impingement syndrome of the shoulder, rotator cuff tear, glenohumeral arthritis) and cardiac ischemia.
Etiology of Cervical Spondylosis
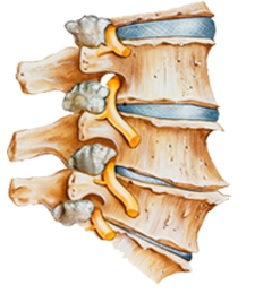 So if cervical spondylosis is an inflammatory degenerative disease of the neck, where is this degeneration occurring? Almost every joint in the neck is made up of three primary pieces: a vertebra, a disc and another vertebrae. These three pieces make up what would look like a peanut butter sandwich. The two slices of bread being the vertebrae and the peanut butter being the disc. What happens is the disc in the middle over time has an increase amount of collagen being produced; this makes it more stable and less mobile with decreased ability to take on loads and compressions. Movement will then not be produced as predominately at the disc itself, but rather on the vertebrae, causing increased mobility, which in turn creates a shear, rotation and traction stress on each vertebrae. This decreased disc height and increased collagen build up allows for approximation of each vertebrae, an increase in the natural cervical lordosis (you begin to present with a greater forward head posture), and possibly buckling of the ligamenum flavum – a column surrounding the neck joints from the front and back.
So if cervical spondylosis is an inflammatory degenerative disease of the neck, where is this degeneration occurring? Almost every joint in the neck is made up of three primary pieces: a vertebra, a disc and another vertebrae. These three pieces make up what would look like a peanut butter sandwich. The two slices of bread being the vertebrae and the peanut butter being the disc. What happens is the disc in the middle over time has an increase amount of collagen being produced; this makes it more stable and less mobile with decreased ability to take on loads and compressions. Movement will then not be produced as predominately at the disc itself, but rather on the vertebrae, causing increased mobility, which in turn creates a shear, rotation and traction stress on each vertebrae. This decreased disc height and increased collagen build up allows for approximation of each vertebrae, an increase in the natural cervical lordosis (you begin to present with a greater forward head posture), and possibly buckling of the ligamenum flavum – a column surrounding the neck joints from the front and back.
Symptoms of Cervical Spondylosis
Now that we know what the condition is and the differential diagnosis of cervical spondylosis, what is the clinical presentation we typically see at glen abbey physiotherapy by our physiotherapist? Usually there is an insidious onset of symptoms with the patient frequently having difficulty determining exactly when the symptoms started, symptoms often follow sustained neck postures and stiffness usuing lasting less then 20 minutes in duration. Pain in the neck is usually described as a dull ache made worse with stress, poor posture, trauma or fatigue. Pain is usually present at end range motions such as doing a blind spot check while driving. The discomfort felt is the neck can be dominated on the left or right side or both equally. If the degeneration of the disc is at a greater extent, it may cause pressure on the nerve above it creating numbness, tingling, burning, coldness, or shooting pain into the arm and/or hand. Headaches are very common with degenerative disc disease and are often reported in the back of the neck just below the skull. Patient’s at Glen Abbey Physiotherapy may also have tender points in the back of their neck and have pain with initiating movement while sitting or lying.
Learn More About Spinal DDD/DJD Here
Physiotherapy Treatment for Cervical Spondylosis
Doctors and surgeons see physiotherapy as the number one conservative management approach to cervical spondylosis. With physiotherapy, patients  often have a decrease in pain, increase in range of motion, improved posture, greater neck strength, a return to their hobbies, activities, and sports that were hindered by their neck limitation. The emphasis of physiotherapy for cervical spondylosis is to avoid aggravating postures or activities, rest in the acute flare-ups because this is the inflammatory stage of healing and needs to be respected in addition to cold or heat therapy and to ensure patients are utilizing the appropriate anti-inflammatory medication as prescribed by a family physician. Physiotherapy at Glen Abbey Physiotherapy goes above and beyond passive treatments. We know that best practice shows that patients have higher rates of recovery when they take an active approach to their rehabilitation from an injury. Therefore our physiotherapists will help you after doing a detailed assessment of your neck and the joints above and below to correctly diagnose your condition. If cervical spondylosis is indeed the diagnosis and cause of your pain and limitations, you can expect an organized team approach treatment program created here at Glen Abbey Physiotherapy. We will utilize, manual therapy techniques, traction, spinal-education, posture education, posture exercises, strength training, stretching techniques, soft tissue massage, create an established home exercise program, heat, ice, interferential current, ultrasound, acupuncture, shockwave, trigger point release, neural mobility techniques and more to help you get the level of care you need dependent on the condition and its stage of healing.
often have a decrease in pain, increase in range of motion, improved posture, greater neck strength, a return to their hobbies, activities, and sports that were hindered by their neck limitation. The emphasis of physiotherapy for cervical spondylosis is to avoid aggravating postures or activities, rest in the acute flare-ups because this is the inflammatory stage of healing and needs to be respected in addition to cold or heat therapy and to ensure patients are utilizing the appropriate anti-inflammatory medication as prescribed by a family physician. Physiotherapy at Glen Abbey Physiotherapy goes above and beyond passive treatments. We know that best practice shows that patients have higher rates of recovery when they take an active approach to their rehabilitation from an injury. Therefore our physiotherapists will help you after doing a detailed assessment of your neck and the joints above and below to correctly diagnose your condition. If cervical spondylosis is indeed the diagnosis and cause of your pain and limitations, you can expect an organized team approach treatment program created here at Glen Abbey Physiotherapy. We will utilize, manual therapy techniques, traction, spinal-education, posture education, posture exercises, strength training, stretching techniques, soft tissue massage, create an established home exercise program, heat, ice, interferential current, ultrasound, acupuncture, shockwave, trigger point release, neural mobility techniques and more to help you get the level of care you need dependent on the condition and its stage of healing.
If you or someone you know are affected by cervical spondylosis or any other neck related injury, be confident in knowing that your registered physiotherapy team here at Glen Abbey Physiotherapy in Oakville is always accepting new patients so we can help the community get back to their hobbies, activities, sports and activities of daily living. Feel free to call us to schedule an appointment with one of our registered physiotherapist to do an orthopaedic examination of your condition.